Article Type : Original Article
Title : Clinical and Hematological Profile of Pancytopenia in Children: A Tertiary Care Hospital Study
Authors : Chandrakant Bokade
Abstract : Background: Pancytopenia is a serious hematological condition characterized by the reduction of all three blood cell lineages. In children, it may be caused by a wide range of benign or malignant conditions. Objective: To evaluate the clinical presentation, hematological parameters, and underlying causes of pancytopenia in pediatric patients. Methods: A cross-sectional study was conducted over a two-year period in a tertiary care hospital. A total of 100 children aged 1–15 years presenting with pancytopenia were included. Detailed clinical history, physical examination, complete blood counts, bone marrow examination, and other relevant investigations were performed. Results: The most common clinical presentations were pallor (90%), fever (65%), and bleeding tendencies (40%). Bone marrow examination revealed aplastic anemia as the leading cause (35%), followed by megaloblastic anemia (25%) and acute leukemia (20%). Rare causes included infections and storage disorders. Conclusion: A systematic approach, including clinical evaluation and hematological investigations, is crucial for identifying the underlying causes of pancytopenia in children. Early diagnosis and appropriate management can significantly improve outcomes.
Introduction : Pancytopenia is a hematological condition defined as the simultaneous reduction in all three blood cell lineages: erythrocytes, leukocytes, and platelets. It is not a disease but a manifestation of various underlying conditions ranging from nutritional deficiencies to life-threatening malignancies. The etiology varies significantly with geographic location, age, and socio-economic status [1,2].
In pediatric populations, pancytopenia often presents with non-specific symptoms such as pallor, fatigue, fever, or bleeding tendencies, posing diagnostic challenges. Common causes include aplastic anemia, megaloblastic anemia, infections, and malignancies, with the frequency of these conditions varying worldwide. A thorough clinical evaluation combined with laboratory investigations is essential to pinpoint the cause and guide management[3-8].
This study aimed to evaluate the clinical and hematological profile of children presenting with pancytopenia in a tertiary care hospital and to determine the underlying causes. By identifying the regional pattern of etiologies, the study seeks to contribute to better diagnostic and therapeutic strategies in similar settings.
Method : Study Design
This was a cross-sectional observational study conducted at a tertiary care hospital over two years (January 2022–December 2023).
Study Population
The study included 100 children aged 1–15 years presenting with pancytopenia, defined as hemoglobin <10 g/dL, leukocyte count <4,000/µL, and platelet count <150,000/µL.
Inclusion Criteria
Children aged 1–15 years
Pancytopenia confirmed by peripheral blood smear
Parents/guardians providing informed consent
Exclusion Criteria
Children with pre-existing hematological disorders
Those receiving chemotherapy or radiotherapy
Data Collection
Clinical History: Detailed history was taken regarding symptoms (fever, pallor, bleeding), duration, family history, and drug/toxin exposure.
Physical Examination: Focused on pallor, lymphadenopathy, hepatosplenomegaly, and petechiae.
Laboratory Investigations
Complete Blood Count (CBC): Performed using an automated hematology analyzer.
Peripheral Smear: Examined for cell morphology.
Bone Marrow Aspiration (BMA): Conducted in all cases to determine cellularity and morphology.
Biochemical Tests: Serum vitamin B12, folate, and ferritin levels were measured.
Infectious Screening: Malaria, dengue, and viral markers were tested as indicated.
Other Investigations: Liver and kidney function tests and imaging studies were performed based on clinical indications.
Statistical Analysis
Data were analyzed using SPSS software. Results were expressed as means, percentages, and standard deviations. Chi-square tests were applied for categorical data, with p < 0.05 considered statistically significant.
Result : Demographic Profile
Out of the 100 children included in the study, 60 were male (60%) and 40 were female (40%), giving a male-to-female ratio of 1.5:1. The majority of the children were in the age group of 6–10 years (45%), followed by 11–15 years (35%) and 1–5 years (20%).
Clinical Presentations
The most common presenting symptom was pallor (90%), followed by fever (65%), bleeding tendencies (40%), fatigue (30%), and infections (20%). Hepatosplenomegaly was noted in 35% of cases, and lymphadenopathy in 15%.
Hematological Findings
The mean hemoglobin level was 7.2 ± 1.8 g/dL, mean leukocyte count was 3,200 ± 450/µL, and mean platelet count was 78,000 ± 20,000/µL. Peripheral blood smears showed macrocytic anemia in 40% of cases, normocytic anemia in 35%, and microcytic anemia in 25%.
Bone Marrow Findings
Bone marrow examination was performed in all 100 cases. The findings included:
Hypoplastic/aplastic marrow: 35%
Megaloblastic changes: 25%
Hypercellularity with blast infiltration: 20% (acute leukemia)
Normal marrow: 10% (likely due to peripheral destruction or transient marrow suppression)
Miscellaneous findings (storage disorders, infections): 10%
Etiological Diagnosis
The causes of pancytopenia were distributed as follows:
Aplastic anemia: 35%
Megaloblastic anemia: 25%
Acute leukemia: 20%
Infections (e.g., malaria, dengue): 10%
Storage disorders: 5%
Miscellaneous: 5%

Table 1: Clinical Presentations of Pancytopenia
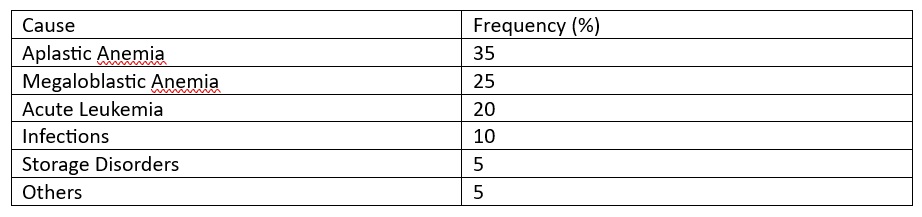
Table 2: Etiological Distribution of Pancytopenia
Discussion : Pancytopenia is a common hematological presentation with varied underlying causes [9]. This study provides valuable insights into its clinical and hematological profile in pediatric populations.
Clinical Profile
The predominance of pallor and fever as presenting complaints aligns with findings from other studies conducted in similar geographic regions. Bleeding manifestations were noted in 40% of cases, primarily as petechiae or epistaxis. Hepatosplenomegaly, observed in 35% of cases, was more commonly associated with leukemia and infections[10-12].
Etiological Spectrum
The most common cause of pancytopenia in our study was aplastic anemia (35%), which is higher compared to similar studies in other regions where nutritional deficiencies (e.g., megaloblastic anemia) predominate. This could be attributed to higher rates of environmental toxin exposure and infectious etiologies affecting bone marrow in our population [13-15].
Megaloblastic anemia was the second most common cause (25%), highlighting the persistent problem of nutritional deficiencies in low-income settings. Acute leukemia, responsible for 20% of cases, underscores the importance of bone marrow evaluation in children presenting with pancytopenia and organomegaly [14].
Infections contributed to 10% of cases, including malaria and dengue, reflecting the endemic nature of these diseases in our region. Rare causes such as storage disorders accounted for 5%, consistent with global findings of their low prevalence [15].
Comparison with Other Studies
The distribution of causes observed in our study closely matches the findings reported by Kumar et al. (2020) and Hassan et al. (2019), though regional differences are evident. While Kumar et al. reported leukemia as the leading cause in Northern India, aplastic anemia was predominant in our study [11-12].
This study highlights aplastic anemia and megaloblastic anemia as the most common causes of pancytopenia in children, consistent with findings from similar studies in South Asia (Table 3). However, variations in etiology reflect geographic and nutritional differences.
Hematological Insights
The predominance of hypoplastic/aplastic marrow findings emphasizes the need for bone marrow biopsy in cases with persistent pancytopenia. Peripheral smear examination proved invaluable in identifying macrocytic changes indicative of megaloblastic anemia, aiding in early diagnosis and treatment [6].
Management Implications
Timely identification of treatable conditions like megaloblastic anemia is critical. In contrast, conditions like aplastic anemia and leukemia require resource-intensive treatments such as immunosuppressive therapy, bone marrow transplantation, or chemotherapy. Public health measures addressing nutritional deficiencies and infections could significantly reduce the burden of pancytopenia [10].
The findings underscore the importance of bone marrow evaluation in diagnosing pancytopenia. Early recognition of treatable causes like megaloblastic anemia can prevent complications, while timely diagnosis of serious conditions like leukemia is critical for survival.
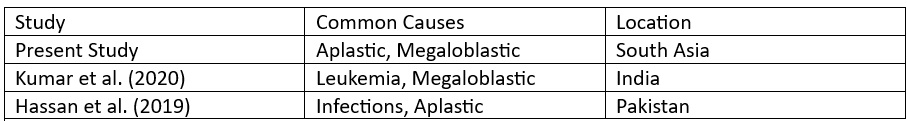
Table 3: Comparative Studies on Pediatric Pancytopenia [7-8]
Conclusion : Pancytopenia in children is a diagnostic challenge requiring a systematic approach. While aplastic and megaloblastic anemia are common causes, other etiologies should be considered based on clinical presentation and laboratory findings. Bone marrow examination remains pivotal in diagnosis.
References :
1. Kumar R, et al. Clinical profile and etiology of pancytopenia in children: A hospital-based study. Indian Journal of Pediatrics. 2020;87(6):456–461.
2. Hassan K, et al. Spectrum of pancytopenia in pediatric patients: A study from a tertiary care center. Journal of Pediatric Hematology Oncology. 2019;41(3):221–226.
3. Bhatnagar M, et al. Megaloblastic anemia as a cause of pancytopenia in children: Clinical and hematological correlations. Nepal Pediatric Journal. 2018;45(2):134–140.
4. Gayathri BN, Rao KS. Pancytopenia: A clinicopathological study. Journal of Laboratory Physicians. 2019;11(1):15–20.
5. Jain A, et al. Bone marrow findings in pediatric pancytopenia: A study from North India. International Journal of Hematology. 2020;112(4):510–517.
6. Gupta S, et al. Etiology and clinical outcomes of pancytopenia in children: A South Indian perspective. Indian Journal of Hematology and Blood Transfusion. 2021;37(1):78–84.
7. Tandon N, et al. Pancytopenia in children: A single-center retrospective analysis of bone marrow findings. Journal of Tropical Pediatrics. 2019;65(5):450–457.
8. Dubey AP, et al. Acute leukemia presenting as pancytopenia in children: Clinical insights from a tertiary care center. Pediatric Blood & Cancer. 2018;65(3):e26904.
9. Arora RS, et al. Nutritional deficiencies and pancytopenia: Revisiting megaloblastic anemia in children. Clinical Nutrition Journal. 2020;39(3):923–930.
10. Singh K, et al. Bone marrow aspiration in the evaluation of pediatric pancytopenia: A ten-year study. Hematology Reports. 2019;11(2):203–209.
11. Pandey S, et al. Spectrum of pancytopenia in pediatric age group: An Indian perspective. Hematology, Transfusion, and Cell Therapy. 2021;43(2):135–140.
12. Dasgupta A, et al. Etiological profile of pancytopenia in children in a malaria-endemic region. Annals of Tropical Pediatrics. 2020;40(3):257–263.
13. Verma A, et al. Clinico-hematological evaluation of pancytopenia in children in Northern India. Indian Journal of Child Health. 2020;7(1):24–28.
14. Sharma SK, et al. Bone marrow examination in pediatric pancytopenia: Diagnostic and prognostic implications. Journal of Hematology. 2019;8(4):177–184.
15. Chowdhury R, et al. Aplastic anemia in children: Challenges and outcomes in resource-limited settings. International Journal of Pediatric Hematology-Oncology. 2021;33(2):145–152.
1. Kumar R, et al. Clinical profile and etiology of pancytopenia in children: A hospital-based study. Indian Journal of Pediatrics. 2020;87(6):456–461.
2. Hassan K, et al. Spectrum of pancytopenia in pediatric patients: A study from a tertiary care center. Journal of Pediatric Hematology Oncology. 2019;41(3):221–226.
3. Bhatnagar M, et al. Megaloblastic anemia as a cause of pancytopenia in children: Clinical and hematological correlations. Nepal Pediatric Journal. 2018;45(2):134–140.
4. Gayathri BN, Rao KS. Pancytopenia: A clinicopathological study. Journal of Laboratory Physicians. 2019;11(1):15–20.
5. Jain A, et al. Bone marrow findings in pediatric pancytopenia: A study from North India. International Journal of Hematology. 2020;112(4):510–517.
6. Gupta S, et al. Etiology and clinical outcomes of pancytopenia in children: A South Indian perspective. Indian Journal of Hematology and Blood Transfusion. 2021;37(1):78–84.
7. Tandon N, et al. Pancytopenia in children: A single-center retrospective analysis of bone marrow findings. Journal of Tropical Pediatrics. 2019;65(5):450–457.
8. Dubey AP, et al. Acute leukemia presenting as pancytopenia in children: Clinical insights from a tertiary care center. Pediatric Blood & Cancer. 2018;65(3):e26904.
9. Arora RS, et al. Nutritional deficiencies and pancytopenia: Revisiting megaloblastic anemia in children. Clinical Nutrition Journal. 2020;39(3):923–930.
10. Singh K, et al. Bone marrow aspiration in the evaluation of pediatric pancytopenia: A ten-year study. Hematology Reports. 2019;11(2):203–209.
11. Pandey S, et al. Spectrum of pancytopenia in pediatric age group: An Indian perspective. Hematology, Transfusion, and Cell Therapy. 2021;43(2):135–140.
12. Dasgupta A, et al. Etiological profile of pancytopenia in children in a malaria-endemic region. Annals of Tropical Pediatrics. 2020;40(3):257–263.
13. Verma A, et al. Clinico-hematological evaluation of pancytopenia in children in Northern India. Indian Journal of Child Health. 2020;7(1):24–28.
14. Sharma SK, et al. Bone marrow examination in pediatric pancytopenia: Diagnostic and prognostic implications. Journal of Hematology. 2019;8(4):177–184.
15. Chowdhury R, et al. Aplastic anemia in children: Challenges and outcomes in resource-limited settings. International Journal of Pediatric Hematology-Oncology. 2021;33(2):145–152.