Article Type : Review Article
Title : Diabetes: Advances in Diagnosis and Treatment
Authors : Amruta Kadbe
Abstract : Diabetes mellitus, a chronic metabolic disorder characterized by hyperglycemia, affects millions globally. The past decade has witnessed remarkable advancements in its diagnosis and treatment. These include improved diagnostic criteria, continuous glucose monitoring (CGM) systems, and innovative therapeutic approaches such as sodium-glucose cotransporter-2 (SGLT2) inhibitors, glucagon-like peptide-1 receptor agonists (GLP-1 RAs), and artificial pancreas technologies. This review explores the latest developments in diabetes management, emphasizing their clinical impact and potential future directions.
Introduction : Diabetes mellitus is a major global health concern, with over 537 million adults affected in 2021, a number projected to rise significantly by 2045. The disease is categorized into type 1 diabetes (T1D), type 2 diabetes (T2D), gestational diabetes mellitus (GDM), and other less common forms. Chronic hyperglycemia in diabetes leads to severe complications, including cardiovascular disease, nephropathy, retinopathy, and neuropathy [1]. Timely diagnosis and effective management are crucial to improving patient outcomes [2]. This article reviews the recent advances in diabetes diagnosis and treatment, highlighting innovations in technology and pharmacology.
Review of Literature : Advances in Diagnosis
1. Enhanced Diagnostic Criteria: [3]
- The adoption of glycated hemoglobin (HbA1c) testing as a diagnostic tool has simplified diabetes diagnosis by reflecting long-term glycemic control.
- Early identification of prediabetes through refined HbA1c thresholds enables timely intervention.
2. Continuous Glucose Monitoring (CGM): [4]
- CGM systems have revolutionized glucose monitoring by providing real-time glucose data, reducing reliance on intermittent finger-stick testing.
- Recent CGM devices, such as the Dexcom G7 and Abbott’s Freestyle Libre 3, offer improved accuracy, user convenience, and integration with digital health platforms.
3. Biomarker Discovery: [4]
- Novel biomarkers, including microRNAs and inflammatory markers, are under investigation for their potential in early diabetes detection and prognosis.
Advances in Treatment [5-9]
1. Pharmacological Innovations:
- Sodium-Glucose Cotransporter-2 (SGLT2) Inhibitors: These drugs, such as empagliflozin and dapagliflozin, not only improve glycemic control but also provide cardiovascular and renal protection.
- Glucagon-Like Peptide-1 Receptor Agonists (GLP-1 RAs): Agents like semaglutide and liraglutide enhance insulin secretion, suppress appetite, and promote weight loss.
- Dual GIP/GLP-1 Receptor Agonists: Tirzepatide, a novel dual agonist, has demonstrated superior efficacy in glycemic and weight management compared to existing therapies.
2. Technological Advancements:
- Artificial Pancreas Systems: Closed-loop insulin delivery systems combine CGM and insulin pumps to automate glucose control, reducing hypoglycemia and hyperglycemia episodes.
- Smart Insulin Pens: These devices track insulin doses and integrate with mobile apps for better diabetes self-management.
3. Adjunct Therapies:
- The use of anti-obesity medications and lifestyle interventions complements traditional diabetes treatments, addressing the metabolic components of the disease.
Discussion : The integration of advanced diagnostic tools and therapeutic strategies has significantly improved diabetes management, reshaping the landscape of care delivery. Continuous glucose monitoring (CGM) systems, for instance, have empowered patients with real-time glucose insights, enabling proactive adjustments to diet, exercise, and medication. This has led to better glycemic control and reduced incidences of severe hypoglycemia, particularly in individuals with type 1 diabetes. Furthermore, the advent of artificial pancreas systems marks a revolutionary step, automating insulin delivery and minimizing human error in disease management [1-5].
Pharmacological advancements, such as SGLT2 inhibitors and GLP-1 receptor agonists, have broadened the therapeutic horizon. Beyond their efficacy in lowering blood glucose, these drugs offer additional benefits, including cardiovascular protection, weight loss, and renal preservation. For example, SGLT2 inhibitors have shown a remarkable ability to reduce hospitalization rates for heart failure, representing a dual benefit for patients with type 2 diabetes and concurrent cardiovascular diseases. Similarly, GLP-1 receptor agonists have proven effective in tackling obesity, a major risk factor for diabetes, thus addressing the disease at its roots [9-11].
To contextualize these advancements, findings from key studies are summarized in Table 1 [7-11].
Despite these advancements, several challenges remain. One of the most pressing issues is the cost associated with modern diabetes management tools and medications. Advanced technologies like CGM and artificial pancreas systems, though highly effective, are often inaccessible to patients in low- and middle-income countries due to financial constraints. Addressing this disparity is crucial for ensuring equitable healthcare [6,7].
Additionally, patient adherence to new therapies and technologies continues to be a challenge. While CGM and insulin pumps offer unparalleled convenience, their adoption requires significant patient education and engagement. Healthcare providers must focus on simplifying these tools and providing comprehensive training to maximize their utility [8,9].
Looking forward, the field of diabetes treatment holds promising avenues. Gene therapy and stem cell-based interventions are being actively explored, offering the potential for long-term remission or even a cure for diabetes. For instance, beta-cell replacement therapy and immunomodulation strategies aim to restore endogenous insulin production in patients with type 1 diabetes. Such approaches, though in early stages, could redefine the standard of care in the coming decades [11].
Interdisciplinary collaboration is also key to addressing the multifaceted nature of diabetes. Integrating endocrinology, cardiology, nephrology, and behavioral health perspectives will enable more holistic patient care. In parallel, leveraging digital health technologies, including telemedicine and mobile health apps, can bridge gaps in access and enhance disease monitoring and management [10].
In summary, while significant strides have been made in diabetes diagnosis and treatment, achieving global impact requires addressing affordability, accessibility, and patient adherence. Continued innovation, supported by robust research and policy efforts, will be essential to tackling the rising burden of diabetes and improving patient outcomes worldwide.
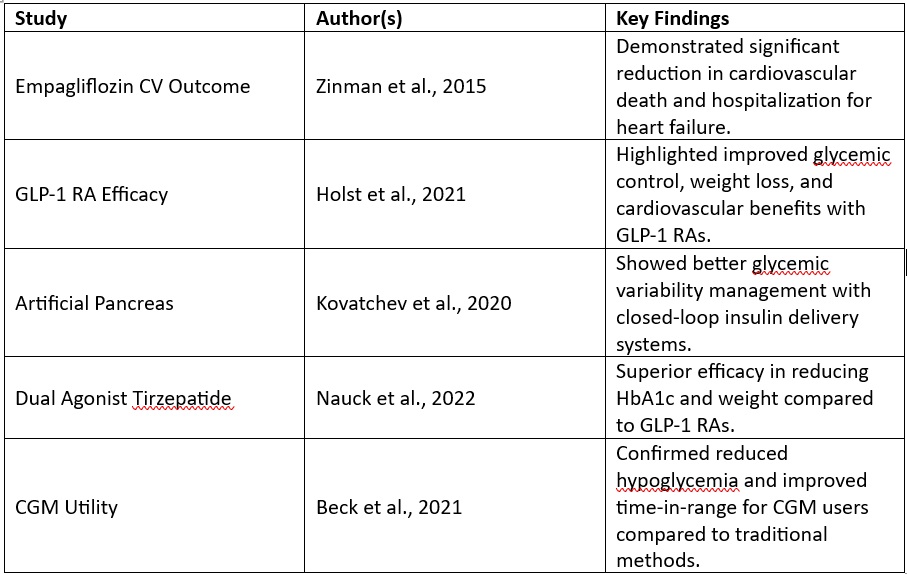
To contextualize these advancements, findings from key studies are summarized in Table 1 [7-11].
Conclusion : The past decade has brought transformative changes in diabetes diagnosis and treatment, improving patient outcomes and quality of life. Continuous innovation, coupled with efforts to enhance accessibility and affordability, will be crucial in addressing the growing diabetes burden worldwide. Interdisciplinary approaches and patient-centric care models will play a pivotal role in the future landscape of diabetes management.
References :
1. International Diabetes Federation. IDF Diabetes Atlas, 10th edition. 2021.
2. American Diabetes Association. Standards of Medical Care in Diabetes—2023.
3. Beck RW, et al. Continuous Glucose Monitoring: Review of an Evolving Technology. Diabetes Care, 2021.
4. Zinman B, et al. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. N Engl J Med, 2015.
5. Davies MJ, et al. Management of Hyperglycemia in Type 2 Diabetes, 2022. Diabetes Care, 2022.
6. Holst JJ, et al. GLP-1 Receptor Agonists in Diabetes Treatment. Nat Rev Endocrinol, 2021.
7. Nauck MA, et al. Tirzepatide: A Novel Dual GIP/GLP-1 Receptor Agonist. Lancet Diabetes Endocrinol, 2022.
8. Kovatchev BP, et al. Artificial Pancreas Systems: Progress and Challenges. Diabetes Technol Ther, 2020.
9. Rajhans K, et al. Smart Insulin Pens: Usability and Efficacy. Diabetes Ther, 2021.
10. Gregg EW, et al. Trends in Diabetes Complications and Mortality. N Engl J Med, 2014.
11. Cosentino F, et al. SGLT2 Inhibitors in Cardiovascular Disease. Eur Heart J, 2020.
1. International Diabetes Federation. IDF Diabetes Atlas, 10th edition. 2021.
2. American Diabetes Association. Standards of Medical Care in Diabetes—2023.
3. Beck RW, et al. Continuous Glucose Monitoring: Review of an Evolving Technology. Diabetes Care, 2021.
4. Zinman B, et al. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. N Engl J Med, 2015.
5. Davies MJ, et al. Management of Hyperglycemia in Type 2 Diabetes, 2022. Diabetes Care, 2022.
6. Holst JJ, et al. GLP-1 Receptor Agonists in Diabetes Treatment. Nat Rev Endocrinol, 2021.
7. Nauck MA, et al. Tirzepatide: A Novel Dual GIP/GLP-1 Receptor Agonist. Lancet Diabetes Endocrinol, 2022.
8. Kovatchev BP, et al. Artificial Pancreas Systems: Progress and Challenges. Diabetes Technol Ther, 2020.
9. Rajhans K, et al. Smart Insulin Pens: Usability and Efficacy. Diabetes Ther, 2021.
10. Gregg EW, et al. Trends in Diabetes Complications and Mortality. N Engl J Med, 2014.
11. Cosentino F, et al. SGLT2 Inhibitors in Cardiovascular Disease. Eur Heart J, 2020.